Effectiveness of deliberate practices versus conventional lecture in trauma training for medical students | BMC Medical Education
On the basis of the results of this study, deliberate practice was significantly more effective than the conventional lecture method in teaching medical students about life-threatening trauma procedures. In this case, the students trained through deliberate practice scored significantly higher on the OSCE and had better overall grades than those under the conventional lecture method did. For example, the mean OSCE score for the deliberate practice group (Group 2) was 69.79, whereas it was 51.38 for the conventional group (Group 1), with a highly significant p value of 0.000002. Moreover, Group 2 had no clear fails and seven good passes, whereas Group 1 had five clear fails and no good passes. These findings highlight not only the efficacy of deliberate practice in improving both the understanding and performance of medical students in critical trauma procedures but also its value in high-stakes and skill-intensive domains such as trauma care.
It is important to note that while both groups received an equal total training duration of 3 h, the deliberate practice group benefited from a distributed learning schedule. This structure provided additional opportunities for iterative feedback, reflection, and readiness assessments, which likely contributed to improved retention and skill acquisition. Educational research consistently supports the notion that spaced learning enhances long-term outcomes compared to massed learning. This staggered approach may have played a significant role in the deliberate practice group’s superior performance. Future studies should explore whether the distribution of training time itself, independent of the teaching method, has an impact on learning effectiveness and skill acquisition.
Overall, this study provides strong evidence for the application of deliberate practice in medical education, especially for teaching life-threatening trauma procedures to medical students. As stated earlier, deliberate practice, as proposed by Ericsson et al. [2] is characterized by focused, goal-oriented, and repetitive practice with immediate feedback, enabling individuals to develop expertise in a specific domain. In this study, the superior performance of the students in Group 2 indicated that structured, purposeful practice effectively increased their skill acquisition. The findings of this study also align with those of Wayne et al. [3] who showed that simulation-based training that incorporated deliberate practice significantly improved the skills of medical residents in advanced cardiac life support (a similar critical procedure). Additionally, Tantiphlachiva et al. [4] demonstrated that deliberate practice greatly enhanced the clinical skills and competencies of medical students, further supporting our findings. While deliberate practice has demonstrated effectiveness, it should be noted that it complements rather than replaces traditional instruction methods. For example, conventional lecture-based education is extremely efficient at providing foundational knowledge and is widely used in medical education to introduce core concepts [5, 6]. In this case, lectures allow instructors to present a broad overview of important topics, offer explanations of complex theories, and clarify students’ questions in real time. When used with deliberate practice, lecture-based instruction can be effective for building an initial understanding before students become engaged in hands-on practice. This is in line with the findings of Issenberg et al. [7] who noted that various instructional methods (e.g., technology-enhanced learning methods) in combination with deliberate practice can be effective for learning in medical education.
The use of ANCOVA in this study was critical in adjusting for potential confounders, such as baseline pretest scores and group characteristics, enhancing the reliability and validity of the findings. By accounting for these variables, ANCOVA allowed for a more accurate comparison of post-test performance between groups, ensuring that the observed differences were primarily attributable to the teaching methods. This statistical adjustment strengthens the study’s conclusions and underscores the effectiveness of deliberate practice in improving learning outcomes. Future studies should continue to use robust statistical methods, such as ANCOVA, to minimize bias and provide more reliable comparisons in educational research.
In this context, Cook et al. [8] indicated that the use of virtual simulations paired with deliberate practice principles can lead to effective learning outcomes that are comparable to those of traditional clinical education. Such simulations can provide a controlled environment in which students are introduced to scenarios before progressing to more intensive, real-world clinical contexts [9, 10]. For example, during trauma procedure training, students in deliberate practice sessions can concentrate on critical components such as airway management, hemorrhage control, and rapid patient assessment. The feedback provided during these sessions can help them identify areas for improvement and refine their techniques [11]. According to McGaghie et al. [12] deliberate practice in simulation-based education has been shown to increase clinical competency and skills retention over time.
The observed improvement in confidence and preparedness among the deliberate practice group is consistent with the principles of deliberate practice, which emphasize iterative feedback, skill refinement, and stepwise mastery. These findings suggest that deliberate practice offers more than just procedural competence—it enhances self-efficacy and readiness to manage high-pressure clinical situations. Confidence and preparedness are critical factors in clinical performance, and the deliberate practice model appears to address these aspects effectively. Future studies could explore the long-term impact of enhanced self-efficacy on clinical decision-making and patient outcomes.
In this study, the deliberate practice sessions also allowed the students to break down complex trauma procedures into smaller, more manageable components, fostering targeted practice and refinement of specific clinical skills [13]. Meanwhile, immediate feedback during these sessions (either from expert facilitators or through self-assessment) enabled the students to pinpoint areas for improvement and adjust their techniques accordingly [14]. This iterative process of targeted practice and feedback allowed the students to continuously challenge themselves and improve their performance. The goal-oriented nature of deliberate practice also helps them maintain their motivation and engagement, which are essential for long-term skills development [2, 11, 15].
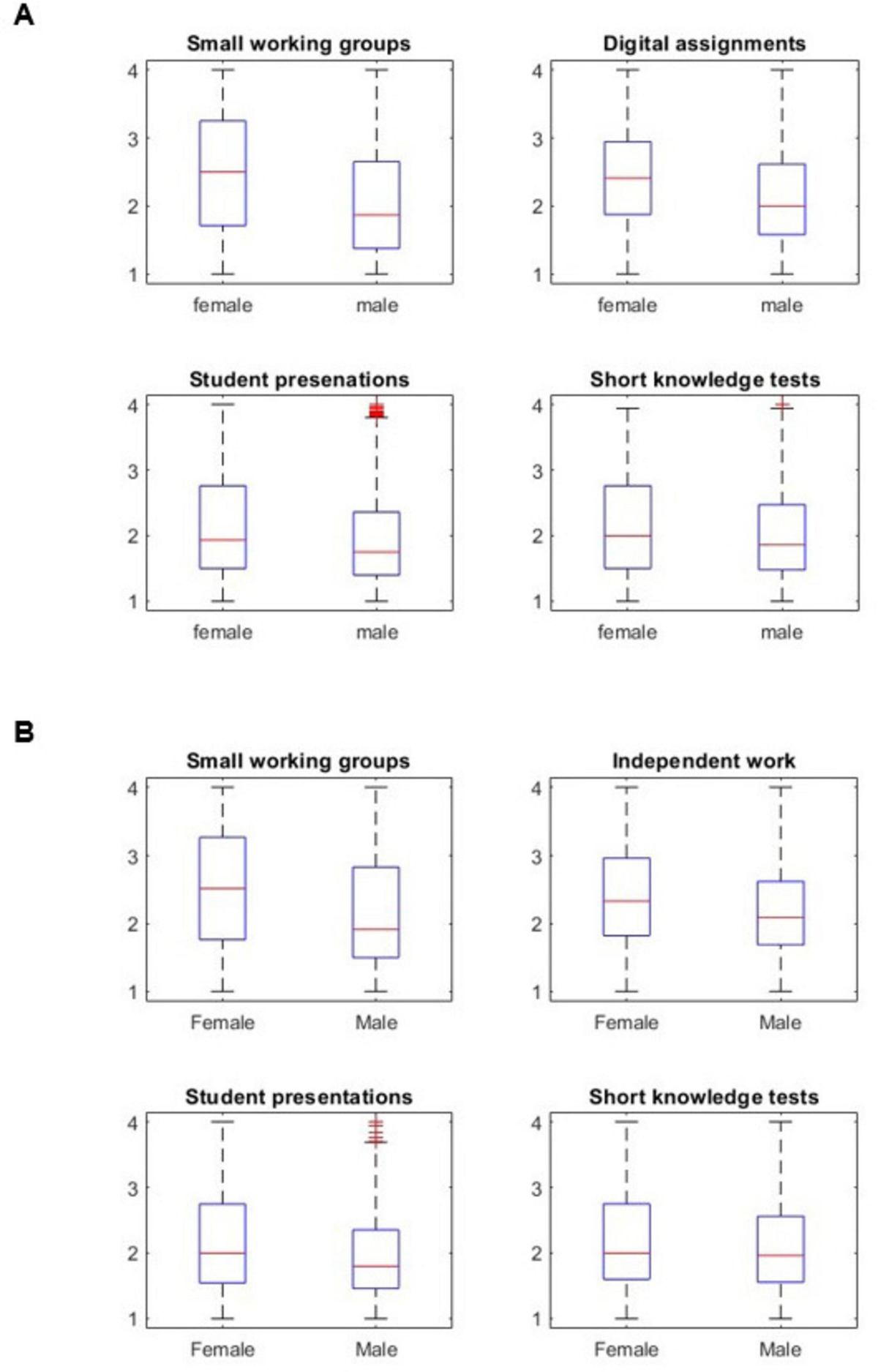
Overall, this study’s strengths include its randomized controlled design, which minimized biases and enhanced the reliability of the results, and the use of the OSCE for assessing competency, which provided a robust measure of medical students’ skills. Moreover, controlling for covariates, such as gender and academic year, through ANCOVA strengthened the validity of the findings.
However, several limitations should be noted. First, the study was conducted within a single medical school, which may limit the generalizability of the findings to other institutions with different educational settings or student populations. Second, the sample size, while adequate for detecting significant differences, was relatively small, and the diversity of participants was limited, which may have further constrained the applicability of the results. Third, the short-term focus of this study did not allow for an assessment of long-term skill retention or the impact of deliberate practice on clinical performance in real-world settings.
Future research should replicate these results in various medical schools with larger, more diverse sample sizes to confirm their generalizability. Longitudinal studies are also needed to evaluate the long-term retention of skills acquired through deliberate practice and their effectiveness in clinical practice. Furthermore, investigating the use of deliberate practice in other areas of medical education can provide a broader understanding of its benefits and limitations. Identifying the specific components of deliberate practice that contribute the most to skill acquisition can also help refine and optimize training programs for medical students on a wider scale.In summary, while deliberate practice has proven to be a powerful tool in developing expertise in medical students, it works best in conjunction with other methods that provide foundational knowledge and situational context. Although this study adds to the literature supporting the use of deliberate practice in medical education, further research is necessary to determine how to best integrate this method with other instructional techniques to optimize learning outcomes in various educational contexts.
link